ESTIV 2016 Posters and Presentations

Representatives from Mattek In Vitro Life Science Laboratories will be attending the ESTIV 2016 annual meeting in Juan-Le-Pins, France. Dr. Helena Kandarova, and Dr. Silvia Letasiova will be presenting several posters on the latest 3D in vitro toxicology innovations, including regulatory toxicology applications, and the new EpiIntestinal small intestinal tissue model. All posters will be displayed from Monday, October 17 to Thursday, October 20. Attending the meeting? Visit us at booth #18. Can’t make it? Request copies of our posters below.
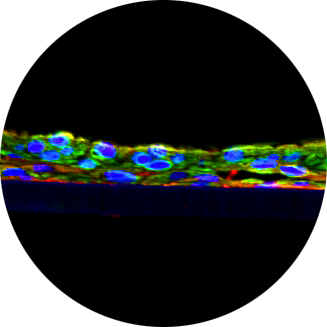
Pre-Validation of human small intestinal tissue model system to screen drug-induced gastrointestinal toxicity and wound healing.
Seyoum Ayehunie, Zachary Stevens, Timothy Landry and Mitchell Klausner
Mattek Corporation, Ashland, MA
Primary human cell-based small intestinal (SMI) tissue models that recapitulate in vivo SMI tissue phenotype, structure and function are critically needed to study gastrointestinal (GI) toxicity, drug permeation, and intestinal restitution. In this study 3D SMI models were used for drug permeation, wound healing, and GI toxicity. Drug permeation studies were performed using 13 drugs that utilize specific transporters (Pgp, BCRP, MRP-2, etc.). GI toxicity was examined using GI toxicants indomethacin and RN38. Outcome measurements include TEER, histology, confocal imaging, and LC-MS/MS analysis for drug permeation. Specific findings include: 1) The SMI tissue models can be cultured for up to 28 days; 2) Dose-dependent toxicity of indomethacin was from TEER values and histological analysis; and 3) Functionally active drug transport (B-to-A transport with efflux ratios >2 fold) for 7 of 13 test compounds was observed. Furthermore, drug efflux transporter inhibitors increased bio availability of drugs while decreasing the efflux ratio. Efflux ratios for talinolol, digoxin, and loperamide (Pgp substrates) were reduced by 45%, 40%, and 60%, respectively, in the presence of the Pgp inhibitor, verapamil. The efflux ratio of the BCRP substrate, nitrofurantoin, was reduced by 63% in the presence of novobiocin, a BCRP inhibitor. Furthermore, tissues cultured in human serum completed the wound healing process 6 days’ post-injury compared to > 10 days for control tissues (no serum). In conclusion, the newly developed SMI tissue models appear to be promising new tools for drug safety, permeation, and wound healing studies.
Request a copy of this poster.
CON4EI: EpiOcular Eye Irritation Test (EIT)
Helena Kandarova1, An R. Van Rompay2, Els Adriaens3, Nathalie Alépée4, Agnieszka Drzewiecka5, Przemyslaw Fochtman5, Katarzyna Gruszka5, Robert Guest6, Gareth Maglennon6, Jane Schofield6, Jamin A. Willoughby7, Sandra Verstraelen1
1Mattek In Vitro Life Sciences Laboratories, Bratislava, Slovakia; 2Flemish Institute for Technological Research (VITO NV), Applied Bio & Molecular Systems, Mol, Belgium; 3Adriaens Consulting bvba, Aalter, Belgium; 4L’Oréal Research & Innovation, Aulnay-sous-Bois, France; 5Institute of Industrial Organic Chemistry Branch Pszczyna, Department of Toxicological Studies, Pszczyna, Poland; 6Envigo, Derbyshire, United Kingdom; 7Cyprotex US, LLC, Kalamazoo, MI 49008, USA
Assessment of the acute eye irritation potential is part of the international regulatory requirements for testing of chemicals. The objective of the CON4EI (CONsortium for in vitro Eye Irritation testing strategy) project is to develop tiered testing strategies for eye irritation assessment for all drivers of classification. For this, a set of 80 reference chemicals (38 liquids and 42 solids) was tested with eight different alternative methods. Here, the results obtained with reconstructed human cornea-like epithelium (RHCE) EpiOcular and the EpiOcular Eye Irritation Test (EIT) -adopted as OECD TG 492 – are shown.
The primary aim of this study was an evaluation of the performance of the test method to discriminate chemicals not requiring classification for serious eye damage/eye irritancy (No Category) from chemicals requiring classification and labelling (Category 1 and 2). In addition, the predictive capacity in terms of in vivo driver of classification was investigated. In a second step, it was investigated whether the EpiOcular EIT can be used as part of a tiered-testing strategy for eye irritation assessment. The chemicals were tested in two independent runs by Mattek IVLSL.
For the EpiOcular EIT, a sensitivity of 96.9% and specificity of 86.7% with an accuracy of 95% was obtained overall and for both runs separately (100% concordance). The results of this study seem promising with regard to the evaluation of inclusion of this test method in an integrated testing strategy for eye irritation assessment.
This research is funded by CEFIC-LRI. We acknowledge Cosmetics Europe for their contribution in chemical selection.
Request a copy of this poster.
Determination of contact sensitization potential of chemicals using in vitro reconstructed normal human epidermal model EpiDerm: impact of the modality of application
Letasiova S.1, Corsini E.2, Galbiati V.2, Kandarova H.1, Lehmeier D.3, Gehrke H.3
1Mattek In Vitro Life Science Laboratories, Bratislava, Slovakia, 2Laboratory of Toxicology, Department of Pharmacological and Biomolecular Sciences, Università degli Studi di Milano, Milan, Italy, 3Eurofins BioPharma Product Testing Munich GmbH, Germany
Assessment of skin sensitization potential has traditionally been conducted in animal models, such as the Mouse Local Lymph Node Assay (LLNA) and the Guinea Pig Maximisation Test (GPMT). However, a growing focus and consensus for minimizing animal use have stimulated the development of in vitro methods to assess skin sensitization. Interleukin-18 (IL-18) release in reconstructed human epidermal models has been identified as a potentially useful endpoint for the identification and classification of skin sensitizing chemicals, including chemicals of low water solubility or stability (1).
The purpose of this study was to investigate the impact of the modality of chemical exposure on the predictive capacity of the assay. EpiDerm tissue viability assessed by MTT assay and IL-18 release assessed by ELISA were evaluated after 24 h topical exposure to test chemicals either impregnated in 8 mm diameter paper filters or directly applied to the surface of EpiDerm. Acetone: olive oil (4:1) was used as vehicle in all cases. A total of five chemicals from 3 different sources were tested. The testing set included 3 senzitizers, namely 2,4-dinitrochlorobenzene, cinnamaldehyde and isoeugenol/eugenol, and 2 non senzitizers, lactic acid and salicylic acid. Four independent dose – response experiments were conducted in 3 laboratories, resulting in correct prediction of the sensitizing potency of test chemicals.
The assessment of IL-18 release using in vitro reconstructed normal human epidermal model EpiDerm appears to be a promising tool for in vitro determination of contact sensitization potential.
Request a copy of this poster.
Assessment of the phototoxicity of three different TiO2 nano-forms using reconstructed human tissue model EpiDerm
Alzbeta Liskova1, Tatiana Milasová2, Sona Jantová1, Vlasta Brezova3 and Helena Kandarova2
1FCHPT, Inst. of Biochemistry, Nutrition and Health Protection, Dep. of Biochemistry and Microbiology, Bratislava, Slovakia, 2Mattek In Vitro Life Science Laboratories, Bratislava, Slovakia, 3FCHPT, Department of Physical Chemistry, Bratislava
Absorption of the solar light by photo-sensitive substances and consequent formation of reactive oxygen species (ROS) and other photo-products may lead to the cellular damage as well as to responses of the immune system. Taken that into the consideration, the determination of phototoxicity of substances absorbing UV and visible spectra of the solar light (VIS) belongs therefore to the basic toxicology tests.
One of the methods used for the determination of phototoxicity is a test based on the use of 3D in vitro reconstructed human skin tissue model-EpiDermTM, the EpiDerm H3D-PT. This test was developed and pre-validated by organization ZEBET already in 1997. The main objective of this work was to verify and determine the phototoxicity and phototoxic potential of the selected reference substances and three different types of TiO2 nanoparticles using the EpiDermTM H3D-PT.
We firstly evaluated and standardized the measurement conditions of the sunlight simulator SOL-500 and verified the sensitivity of the EpiDermTM tissues towards UV/VIS light. Next, we evaluated correct prediction of phototoxicity of the EpiDermTM H3D-PT using six reference substances, of which four were known phototoxins (chlorpromazine hydrochloride, two types of bergamot oil and anthracene) and two compounds were UV-absorbing, but without phototoxic potential (cinnamaldehyde, p-aminobenzoic acid). Finally, we have used this method to predict the phototoxicity of three different types of titanium dioxide (P25 AEROXID, Eusolex T-2000, TIG-115).
Based on the results obtained in this work, we conclude that the EpiDermTM H3D-PT is a reliable test for the detection of phototoxicity and prediction of the phototoxic potential of selected substances. This conclusion is supported by the fact that during the measurements we obtained the same or better results as published by Liebsch et al. (1997). Phototoxicity of TiO2 has not been demonstrated in any of the three samples tested. This is because TiO2 nanoparticles do not penetrate deep enough into the epidermis to cause cytotoxicity by irradiation with UVA/VIS.
Request a copy of this poster.
Use of ECVAM-Validated EpiDerm Skin Corrosion Test (EpiDermSCT) for Sub-Categorization According to the UN GHS
Letasiova, Silvia1, Kandarova, Helena1, Hayden, Patrick2, Klausner, Mitchell2
1Mattek In Vitro Life Science Laboratories, Mlynské Nivy 73, 821 05 Bratislava, Slovak Republic, 2Mattek Corporation, 200 Homer Avenue, 01721 Ashland, MA, USA
Skin corrosion refers to the production of irreversible damage to the skin. OECD adopted four reconstructed human skin model assays for predicting skin corrosion in vitro (OECD TG 431). The guideline, however, does not yet fully satisfy international labelling guidelines for transport of dangerous goods.
The UN-GHS utilizes 3 corrosion sub-categories (1A-very dangerous,1B-medium danger and 1C-minor danger). Labelling a chemical as 1A has important consequences for transport and animal tests are still utilized for assessing the packaging subclasses. An in vitro method that could discriminate at least between the 1A vs 1B/1C classes would therefore have a substantial impact on reducing animal tests for this purpose.
The current study evaluates prediction of the sub-classes using the EpiDerm SCT and 80 chemicals selected by the OECD expert group for skin irritation and corrosion. Using tiered classification strategy, sensitivity for class 1A was 86% using 3 min exposure time-point. None of 1A chemicals were under-predicted as NC. Specificity for NC chemicals was 74%. As demonstrated, the EpiDerm SCT allows a partial sub-classification of corrosives into sub-category 1A, 1B/1C,and NC. Adoption of the new prediction model based on a 3 min endpoint into the validated EpiDerm SCT and the OECD TG 431 will allow identification of severely corrosive substances without the use of animals.
Request a copy of this poster.
Development, Optimization and Validation of an in vitro Skin Irritation Test for Medical Devices Using the Reconstructed Human Tissue Model EpiDerm
Kandarova, Helena1,4; Willoughby, Jamin A.2; de Jong, Wim H.3; Bachelor, Michael A.4; Letasiova, Silvia1; Milasova, Tatiana1; Breyfogle, Bridget4; de la Fonteyne, Liset3; Haishima, Yuji5; Coleman, Kelly P.6
1Mattek IVLSL, Bratislava, Slovakia, 2Cyprotex US LLC, Kalamazoo, MI, United States, 3RIVM, Bilthoven, Netherlands, 4Mattek Corporation, Ashland, MA, United States, 5Division of Medical Devices – NIHS, Tokyo, Japan, 6Medtronic, Inc, Minneapolis, MN, United States.
Assessment of dermal irritation is an essential component of the safety evaluation of medical devices. Reconstructed human epidermis (RhE) models have replaced rabbit skin irritation testing for neat chemicals (OECD TG 439). However, medical device (MD) extracts are dilute solutions with low irritation potential, therefore the validated RhE-methods needed to be modified to reflect needs of ISO 10993.
A protocol employing RhE EpiDerm was optimized in 2013 using known irritants and spiked polymers (Casas et al., TIV, 2013).
In 2014, a second laboratory assessed the transferability of the assay. Two additional exposure times were tested along with other medical device materials. After the successful transfer and standardization of the protocol, nine EU and USA laboratories were trained in the use of the protocol in the preparation for the validation. All laboratories produced data with almost 100% agreement of predictions for the selected references.
Two of the laboratories performed additional tests with heat-pressed PVC sheets spiked with Genapol X-080 (Y-4 polymer), Vicryl suture, and polymers spiked with heptanoic acid and sodium dodecyl sulfate. All materials were extracted for 24 or 72 hours in both saline and sesame oil at either 37°C.
Significant irritation responses were detected for Y-4 under all conditions. These results were consistent with those reported by other research groups involved in the upcoming validation study. Vicryl suture was negative and spiked polymers were either positive or negative dependent on the extraction solvent.
We conclude that a modified RhE skin irritation test has the potential to address the skin irritation potential of the medical devices, however, standardization and focus on the technical issues is essential for accurate prediction. Round Robin validation of the Skin irritation test in vitro for assessment of Medical devices extracts has started in March 2016.