Eurotox 2019 in Helsinki
Mattek scientists from the US and EU will be attending, sponsoring and presenting posters at Eurotox 2019 in Helsinki Finland. Read more to see what they’ve been working on and request copies of their presentations.
We’re proud to be Bronze Sponsors of Eurotox 2019
Meet our team at Booth #5
We’d love to chat: Schedule a Meeting
Poster Presentations:
All posters will be exhibited in the P06 In Vitro Testing Session on Monday, September 9, during congress breaks
ALT4EI: Evaluation of eye irritating potential of 59 chemicals using EpiOcular™ time-to-toxicity (EpiOcular ET-50) neat and dilution protocols (Abstract ID: 530)
Silvia Letasiova1, Helena Kandarova1, Els Adriaens 2, Sandra Verstraelen3, and An R. Van Rompay3
1 Mattek In Vitro Life Science Laboratories, Mlynske Nivy 73, Bratislava, Slovakia
2 Adriaens Consulting BVBA, Bellemdorpweg 95, 9981 Aalter, Belgium.
3 VITO NV, UNI Health, Boeretang 200, 2400 Mol, Belgium
Abstract
Evaluation of the acute eye irritation potential is part of the international regulatory requirements for testing of chemicals. The objective of the ALT4EI (ALTernatives for Eye Irritation) project was to confirm the testing strategy developed in the CON4EI (CONsortium for in vitro Eye Irritation testing strategy) project. These projects focussed on the development of tiered testing strategies for eye irritation assessment for all drivers of classification and evaluation of whether the test methods can discriminate chemicals not requiring classification for serious eye damage/eye irritancy (No Category) from chemicals requiring classification and labelling for Category 1 (Cat 1) and Category 2 (Cat 2). A new set of 59 chemicals (41 liquids: (un)diluted, and 18 solids) was tested using the reconstructed human cornea-like epithelium (RhCE), EpiOcular, in two EpiOcular time-to-toxicity Tests (Neat and Dilution ET-50 protocols). The set of chemicals contained 32 chemicals not requiring classification (No Cat) and 27 chemicals requiring classification (16 Cat 2 and 11 Cat 1). The chemicals were tested blinded in two independent runs by Mattek In Vitro Life Science Laboratories. In this study, a testing strategy to achieve optimal prediction for all three classes that was developed in CON4EI project (which combines the most predictive time-points of both protocols and which tests liquids and solids separately) was used. Using the CON4EI testing strategy, we were able to identify correctly 63,6 % of the Cat 1 chemicals, 56,6 % of the Cat 2, and 76,6 % of No Cat chemicals. Reproducibility between both runs was 88,7 %. The combination of the EpiOcular ET-50 neat and dilution protocols seem to be promising in an integrated testing strategy (ITS) for eye irritation assessment.
Keywords: ALT4EI, EpiOcular ET-50, ocular irritation assay, in vitro, testing strategy
Request a Copy
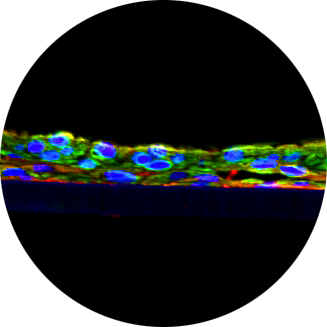
Drug Permeability and Safety Screening Using a Reproducible In Vitro 3D-Human Small Intestinal Tissue Model (Abstract ID: 946) P06 In Vitro Testing
Markus2, T. Landry1, Z. Stevens1, M. Klausner1, P. Hayden1, S. Ayehunie1
1 Mattek Corporation, Ashland, Massachusetts, United States of America
2 Mattek In Vitro Life Science Laboratories, Bratislava, Slovakia
Abstract
Reliable and highly reproducible in vitro models of the small intestine are paramount in predicting of safety and bioavailability of compounds intended for oral administration. Here we describe reproducible production of a recently developed in vitro 3D-human small intestinal (SMI) microtissue model and its use in predicting the drug absorption. Characterization of the microtissues included evaluation of structural features, barrier properties, and expression of drug transporters and drug-metabolizing enzymes. The quality and reproducibility of tissue production were compared in two independent production facilities (Mattek, Ashland, MA, USA and IVLSL, Bratislava, Slovakia) by measuring TEER and Lucifer Yellow (LY) leakage. To evaluate the suitability of the microtissues for drug absorption, the apparent permeability coefficient (Papp) values for a panel of benchmark drugs with known human absorption values were measured. Drug-drug interactions were examined using drugs known to be substrates or inhibitors of efflux transporters. Results showed that tissues are highly reproducible with physiological TEER values averaging 146.4±20.8 Ω*cm2 (% CV=14.2%) in the USA (N=128 lots) and 162.6±10.2 Ω*cm2 in Slovakia (N=60 lots) facilities. The real-time PCR analysis revealed that microtissues expressed all tested drug transporters and metabolizing enzymes known to be present in vivo. Drug permeation analysis with 18 selected drugs showed that the intestinal microtissues could discriminate between low and high permeability drugs with 94% accuracy. The in vitro Papp values correlated well with human absorption data (r2 = 0.91), while correlation of CaCo2 results showed r2 = 0.71. SMI microtissues show an active efflux transport as when exposed to substrates of ABC pumps, the resulting drug efflux ratios were > 2.0. Moreover, the addition of efflux transporter inhibitors reduced the drug efflux ratio while increasing the bioavailability of the test drugs, providing further evidence of ABC transporter activity. In conclusion, the SMI microtissues appear to be a promising tool for predicting the safety and bioavailability of orally administered drugs.
Use of Organotypic Small Intestinal Tissue Model for Drug-Induced Gastrointestinal Toxicity Studies (Abstract ID: 907) P06 In Vitro Testing
Seyoum Ayehunie1, Zachary Stevens1, Timothy Landry1, Jan Markus2, Alex Armento1, Mitchell Klausner1, and Patrick Hayden1
1 Mattek Corporation, Ashland, MA, USA
2 Mattek In Vitro Life Science Laboratories, Bratislava, Slovakia
Abstract
The objective of the study is to evaluate the utility of a 3D primary human cell-based small intestinal tissues as an investigational tool for drug-induced gastrointestinal (GI) toxicity. GI toxicity often leads to late-stage drug attrition or chronic diseases. Animal models have been widely applied for assessing GI toxicity as preclinical test models, however, animal models are expensive, time-consuming and less translatable to human conditions. Hence, in vitro models are needed to guide the design of molecules or dosing schedules that mitigate safety risks in humans. Here we tested a) N=5 therapeutic compounds for which anima toxicity studies were not predictive of human toxicities. Drugs that were well tolerated (N=3) or known to cause gut irritation/toxicity (N=2) in humans were used as negative and positive controls, respectively. MTT viability and tissue barrier integrity as measured by transepithelial electrical resistance (TEER) were used as endpoints to monitor drug-induced GI toxicity. The results showed that the SMI system detected drug-induced disruption of intestinal barrier function (TEER) in 5/5 problematic drugs with human GI toxicity at concentrations within or below 30x clinical exposure levels. Importantly, the SMI system showed no effect within 1,000x clinical exposure levels for the three negative controls. We found that TEER measurement was more sensitive than the MTT viability assay. Using the TEER endpoint we also assessed and confirmed gut barrier dysfunction by two known GI toxicants SN38 (metabolite of Irinotecan) and Ibuprofen in a time and concentration-dependent manner. Irinotecan, the parental drug for SN38 did not induce toxicity on the intestinal tissue model. Changes in barrier integrity as measured by TEER was found to be a valuable endpoint as a predictive tool to assess the toxicity of clinically relevant drug exposures. In conclusion, the in vitro human primary cell-based small intestinal tissue model may serve as a promising tool to predict GI toxicity in humans.
Development of a Subacute 28-Day Respiratory Toxicity Assay Using an In Vitro Human Airway Model (Abstract ID: 957) P06 In Vitro Testing
George R. Jackson, Jr., Michelle Debatis, Mitchell Klausner, Anna G. Maione, Patrick J. Hayden
Mattek Corporation, Ashland, MA, USA
Abstract
Knowledge of subacute (28-day) respiratory toxicity potential is an important component of establishing safe use of chemicals and consumer products. The current work describes efforts to develop an alternative, non-animal method for determining subacute respiratory toxicity using the EpiAirway™ in vitro human airway model. Initial acute toxicity experiments were conducted by exposing EpiAirway tissues to four concentrations of test chemicals via apical application using either aqueous or corn oil vehicles for three hours. After exposure, the test chemicals were rinsed off and the tissues were incubated for an additional 21 hours. An IC75 concentration (concentration required to reduce the endpoint value to 75% of vehicle exposed controls) was determined from the dose-response data using barrier function (determined by measuring transepithelial electrical resistance (TEER)) and tissue viability (MTT assay) as endpoints. Based on the determined acute IC75 value, EpiAirway tissues were exposed to additional serial dilutions of the test chemicals, using the IC75 as the baseline dose. Tissues were apically exposed for three hours, followed by rinsing, every Monday, Wednesday and Friday, with TEER measured prior to each dose application. Experiments were continued for at least 30 days to determine no-observed-adverse-effect level (NOAEL) doses. Rank ordering of NOAEL levels obtained for 8 chemicals was as follows: formaldehyde << butyl amine < oxalic acid << vinyl acetate < morpholine < methyl methacrylate << dimethylacetamide < ethanol. Expansion of the data set to include additional chemicals of different classes, chemical structures and physical properties is ongoing. These results indicate that in vitro airway tissue models using TEER as a convenient non-destructive endpoint are a promising alternative to animal tests for assessment of subacute 28-day respiratory toxicity and NOAELs. With further in vivo correlation and validation, this test may be a useful non-animal alternative for determining safe human subacute exposure levels for inhaled chemicals.