Mattek Presenting Posters and Talks at the 2nd Annual Pan-American Conference for Alternative Methods


Mattek Corporation will be attending the 2nd Annual Pan-American Conference for Alternative Methods in Rio de Janiero, Brazil, from August 23rd to August 24th. The inaugural conference occurred in Baltimore in 2016  and successfully brought together organizations from North, Central, and South America to present alternatives to animal testing methods and discuss future technology collaboration furthering scientific discovery. Mattek’s Dr. Patrick Hayden will be presenting posters and talks about our innovative and industry-leading products at this year’s meeting.
and successfully brought together organizations from North, Central, and South America to present alternatives to animal testing methods and discuss future technology collaboration furthering scientific discovery. Mattek’s Dr. Patrick Hayden will be presenting posters and talks about our innovative and industry-leading products at this year’s meeting.
View Our Posters:
Performance of the OECD Accepted In Vitro Skin Irritation Test (SIT) using the EpiDerm Reconstructed Human Epidermal (RHE) Model
Helena Kandárová (Mattek IVLSL); Patrick Hayden (Mattek Corp.); Mitchell Klausner (Mattek Corp.)
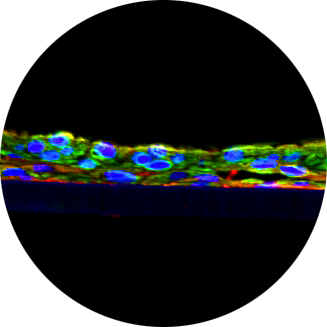
The EpiDerm Skin Irritation test (EpiDerm SIT) was developed, validated by ECVAM and implemented according to OECD test guideline 439 for in vitro skin irritation testing of chemicals, including cosmetic and pharmaceutical ingredients. The EpiDerm SIT utilizes the 3D in vitro reconstructed human epidermal (RHE) model EpiDerm and allows for discrimination between irritants of GHS category 2 and non-irritants. The test is performed over the course of a 4 day time period, consisting of pre-incubation, 60-minute exposure, 42-hour post-incubation and MTT viability assay. After tissue receipt and overnight pre-incubation (Day 0), tissues are topically exposed to the test chemicals (Day 1), which can be liquid, semi-solid, solid or wax. Three tissues are used for each test chemical, as well as for the positive control (5% aq. SDS solution), and a negative control (DPBS). Chemical exposure lasts for 60 minutes, 35 min of which the tissues are kept in an incubator at 37°C. The test substances are then removed from the tissue surface by an extensive washing procedure. The tissue inserts are blotted and transferred to fresh medium. After a 24 hr incubation period (Day 2), the medium is exchanged. The medium can be saved for further analysis of cytokines or other endpoints of interest. After the medium exchange, tissues are incubated for an additional 18 hours. At the end of the entire 42h post-incubation (day 3), the tissues are transferred into yellow MTT solution and incubated for 3 hours. The resultant purple-blue formazan salt, formed mainly by mitochondrial metabolism, is extracted for 2 hours using isopropanol. The optical density of the extracted formazan is determined using a spectrophotometer. A chemical is classified as an irritant if the tissue viability relative to the negative control treated tissues is reduced below 50%. The EpiDerm SIT test is accepted as a full replacement of the in vivo rabbit skin irritation test for hazard identification and labeling of chemicals in line with EU and GHS regulations.
Use of In Vitro Human Intestinal Microtissues as Relevant Models for Drug Permeation and Metabolism in the Gut
Seyoum Ayehunie (Mattek Corp.); Timothy Landry (Mattek Corp.); Zachary Stevens (Mattek Corp.); Mitchell Klausner (Mattek Corp.); and Patrick Hayden (Mattek Corp.)
The goal of this study was to validate the relevance of an in vitro organotypic human small intestinal (SMI) microtissue model (EpiIntestinal) for predicting intestinal drug safety, permeability and metabolism. Permeability coefficients of 16 drugs for which in vivo data are available were evaluated. Toxicity was assessed using transepithelial electrical resistance, MTT viability, and Lucifer Yellow leakage assays. Bioavailability or efflux transport of drugs was analyzed using LC-MS/MS. The metabolic activity of the SMI microtissue model was also assessed and metabolites were analyzed using LC/MS or using isozyme-specific fluorogenic CYP450 substrates. The SMI microtissue model categorized the test drugs as high permeability and low permeability with a sensitivity of 100%, specificity of 89%, and accuracy of 94% compared to historical human absorption data. Efflux transporter Inhibitors increased bioavailability and decreased efflux ratio. Efflux ratios for substrates talinolol, digoxin and loperamide were reduced by 45%, 40%, and 60%, respectively, in the presence of the P-gp inhibitor verapamil. The efflux ratio of nitrofurantoin (BCRP substrate) was reduced by 63% in the presence of the BCRP inhibitor, novobiocin. Midazolam (CPY3A substrate) was metabolized (6.5% conversion) by the SMI microtissue model. Furthermore, Metabolism by CYP2C9, CYP2C19, CYP3A4, and CYP3A5 was observed using isozyme-specific fluorogenic CYP450 substrates. In conclusion, the SMI microtissue model appears to be a promising new tool for evaluation of drug safety, permeability, and metabolism.
Attend Our Talks:
EpiOcular Eye Irritation Test (EpiOcular-EIT) for identification of materials not requiring classification and labeling for eye irritation or serious eye damage
Yulia Kaluzhny (Mattek), Helena Kandárová (Mattek IVLSL), Laurence d’Argembeau-Thornton (Mattek), Thoa Truong (Mattek), Paul Kearney (Mattek), Patrick Hayden (Mattek), and Mitchell Klausner (Mattek)
Assessment of eye irritation hazard has long been a core requirement for international chemicals regulatory legislation. Implementation of the 7th Amendment to the EU Cosmetics Directive, international REACH legislation, and the Frank R. Lautenberg Chemical Safety for the 21st Century Act has heightened the need for predictive in vitro ocular test methods. To address this demand, the in vitro non-animal EpiOcular Eye Irritation Test (EpiOcular-EIT) was developed, validated and implemented as an OECD-approved test guideline (TG 492). The EpiOcular-EIT test is applicable to a wide range of chemicals, including substances and mixtures, solids, liquids, semi-solids, and waxes. The test utilizes EpiOcular, a three dimensional reconstructed human cornea-like epithelial (RhCE) tissue model. EpiOcular is cultured on cell culture inserts and forms a multi-layered structure which closely resembles the histological, morphological, and physiological properties of the human corneal epithelium. The EpiOcular-EIT protocol is able to discriminate between ocular irritant/corrosive materials (GHS Categories 1/2) and those that require no labeling (GHS No Category). The test utilizes two separate protocols, one designed for liquid chemicals and a second, related protocol for solids. The EpiOcular-EIT prediction model uses a single exposure period (30 min for liquids, 6 hours for solids) and a single cut-off (60%) in tissue viability, which is determined by the MTT assay. Based on the results from 83 chemicals (44 liquids and 39 solids) EpiOcular-EIT achieved 95.5/68.2/81.8% sensitivity/specificity/accuracy (SS&A) for liquids, 100.0/68.4/84.6% SS&A for solids, and 97.6/68.3/83.1% for overall SS&A. The EpiOcular-EIT, together with EpiOcular’s long history of reproducibility, provide an important model for addressing and supporting international regulatory labeling requirements according to the current UN GHS legislation for testing of potential ocular irritants.
Pre-Validation of an Acute Inhalation Toxicity Assay Using the EpiAirway In Vitro Human Airway Model
George R. Jackson, Jr. (Mattek Corp.); Michelle Debatis (Mattek Corp.); Anna G. Maione (Mattek Corp.); Patrick J. Hayden (Mattek Corp.)
Knowledge of acute inhalation toxicity potential is important for establishing safe use of chemicals and consumer products. Inhalation toxicity testing and classification procedures currently accepted within worldwide government regulatory systems rely primarily on tests conducted in animals. The goal of the current work was to develop and pre-validate a non-animal (in vitro) test for determining acute inhalation toxicity using the EpiAirway™ in vitro human airway model as a potential alternative for currently accepted animal tests. The in vitro test method exposes EpiAirway tissues to test chemicals for 3 hrs, followed by measurement of tissue viability as the test endpoint. Fifty-nine chemicals covering a broad range of toxicity classes, chemical structures and physical properties were evaluated. The in vitro toxicity data was utilized to establish a prediction model to classify the chemicals into categories corresponding to currently accepted GHS and EPA systems. The EpiAirway IC75 prediction model identified in vivo rat based GHS Acute Inhalation Toxicity Category 1-2 and EPA Acute Inhalation Toxicity Category I-II chemicals with 100% sensitivity, and specificity of 43.1% and 50.0%, for GHS and EPA acute inhalation toxicity systems, respectively. The sensitivity and specificity of the EpiAirway prediction model for identifying GHS Specific Target Organ Toxicity – Single Exposure (STOT-SE) Category 1 human toxicants was 75.0% and 56.5%, respectively. Corrosivity, electrophilic and oxidative reactivity appear to be the predominant mechanisms of toxicity for the most highly toxic chemicals. These results indicate that the EpiAirway test is a promising alternative to the currently accepted animal tests for acute inhalation toxicity.