Meet Mattek in Chicago for SID 2019


Visit our booth and poster presentations
Mattek will be attending, exhibiting, and presenting at this year’s Society for Investigative Dermatology (SID) 2019 Annual Meeting in Chicago, IL. The 77th annual meeting will take place at the Hilton Chicago in Chicago, IL, from May 8 – May 11. Visit our staff at Booth #113 and don’t miss our poster presentations of our latest research. Download our posters below to learn more about our skin disease models including Psoriasis and our new Atopic Dermatitis model.
Are you also attending SID? Chat with our staff to learn more about reliable cosmetic testing and our new skin disease models.
Schedule a Meeting
View our posters
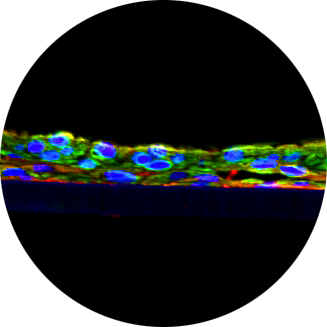
Induction of an atopic dermatitis-like phenotype in a full-thickness in vitro human skin model
Patrick Hayden, Seyoum Ayehunie, Jonathan Oldach, Mitchell Klausner. | Mattek Corporation, Ashland, MA, United States
Reference ID: 726 Presentation time: Poster Session 2 Friday, May 10, 2019 @ 11:15 am – 1:15 pm
Abstract: Atopic dermatitis (AD) is the most common inflammatory disease of the skin and is characterized by defects in keratinocyte differentiation and skin barrier dysfunction. The goal of the current work is to create an in vitro AD model for use in basic research and therapeutic development. To create the model, the EpiDermFT in vitro full-thickness human skin model was treated with a cocktail of Th2 cytokines to induce an AD phenotype. Following cytokine treatment, significant changes in differentiation markers, chemokines involved in T-cell recruitment, and skin barrier integrity were observed, closely resembling features found in AD skin in vivo. Specifically, differentiation markers such as keratin 1, keratin 10, involucrin and filaggrin were downregulated, and chemokines such as CCL3, CCL5, and CCL27 were upregulated at both the gene and protein level. Histological analysis revealed a thinner stratum corneum and spongiosis. Treatment with a corticosteroid, clobetasol proprionate, was able to partially restore normal epidermal morphology and reverse expression of the AD biomarkers. These findings demonstrate that the model is consistent with key hallmarks of AD, and that it may be a useful model for testing therapeutic formulations.
Get a Copy
T-cell cytokines (IL-17 and IFN-N3) exacerbates innate immune responses in an organotypic human psoriasis tissue model.
Seyoum Ayehunie, Timothy Landry, Cristy Hedin, Alex Armento, Patrick Hayden, Mitchell Klausner. | Mattek Corporation, Ashland, MA, United States
Reference ID: 523 Presentation time: Poster Session I Thursday, May 9, 2019 @ 10:45 am – 12:45 pm
Abstract: Psoriasis is a chronic inflammatory immune-mediated skin disease marked by hyperproliferation, abnormal keratinocyte (KC) differentiation, and leukocyte infiltration. Research into the pathogenesis of psoriasis has been hampered by the lack of in vitro models that provides insight into the mechanisms of disease or efficacy of therapeutics. Species differences between existing rodent models and humans raises major translational issues. Since T cells, particularly Th17 cells) are key players in psoriasis, anti-IL-17A antibodies such as Secukinumab have been developed as therapeutics. Based on these scientific developments, we investigated the role of IL-17 alone or in combination with IFN-N3 (Th1 cytokines) in exacerbating inflammatory innate immune responses using a reconstructed 3D human psoriatic tissue model. Normal human keratinocytes (KC) and psoriatic fibroblasts from lesional sites were harvested from primary tissues and cultured using defined serum-free medium to form a highly differentiated 3-dimensional tissue model. The reconstructed psoriatic tissue model was exposed to IL-17 / IFN-N3 for up to 96 hr (4X exposure). The results showed that: 1) IL-17 increases the Th-17 cell and dendritic cells/monocytes chemoattractant (CCL-20), the neutrophil chemoatractant (IL-8), and the anti microbial peptides (HBD2 and elafin (PI3) by 2-7-fold. 2) IFN-N3 induces overexpression of the chemoattractant for activated T cells (CXCL11), IL-8, and TNF-N1 by 2-324-fold. 3). IL-17 and IFN-N3 exacerbate inflammation synergistically by increasing expression levels of the neutrophil chemoattractants (CXCL5, IL-8, IL-6), HBD2, PI3, and TNF-N1 by > 3-fold. In conclusion, we show that a self-sustaining inflammatory feedback loop that involves T-cell cytokines (IL-17, IFN- N3) and KC/fibroblast-derived CCL20, CXCL5, HBD2, PI3, IL-8, and IL-6 is established. Thus, level of innate immune responses such as CCL-20, IL-8, IL-6, and CXCL-5 following treatment can serve as surrogate markers to examine novel biologic therapies.
Get a Copy