Correlation of In Vitro and In Vivo Skin Irritation Assays in Medical Devices: A Case Study
- TR Number: 984
- Authors: C. D. Christensen, S. M. Street, S. K. Mishra, D. E. Oseid, J. M. Martinez, and W. V. Christian
- Materials Tested: synthetic polymers, metal, alloys, implant, silver, copper/zinc, sesame oil, saline
Biocompatibility testing is moving away from animal-based assays in favor of technologically advanced and reliable in silico and in vitro alternative approaches. While irritation has traditionally been assessed in a rabbit animal model, validated reconstructed human epidermis(RhE) models have been introduced in ISO 10993-23:2021. This standard describes a step-wise approach to evaluating the potential for medical devices to cause irritation, most notably deviating from the prior approach described in ISO 10993-10:2010 by calling for in vitro testing prior to in vivo testing.
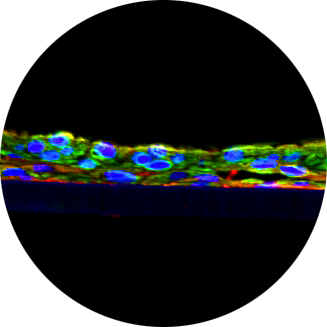
As described in ISO 10993-23:2021, the RhE model is made of human-derived epidermal keratinocytes cultured to form a multi-layered, highly differentiated model of the human epidermis(Fig.1). Structurally, they are arranged in patterns analogous to those in vivo with basal, spinous, and granular layers and a multi-layered stratum corneum with intercellular lamellar lipid layers. The test article is extracted as described in ISO 10993-12:2021 with polar and non-polar solvents. The tissue is incubated with the extract for several hours, then rinsed and dried prior to incubating the tissue with MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide). Cell viability is determined based on a colorimetric assay where cellular uptake (cytotoxicity) of MTT and conversion to a purple formazan salt is quantitatively measured after extraction from the tissues.
Several studies document the development of the RhE model’s application for use in medical device testing and its reliability for correctly identifying known irritants (Casas et al.,2013, Kandárová et al.,2018a, Kandárová et al.,2018b,Olsen et al.,2018). Pellevosin et al.(2018) used the RhE model to evaluate poly vinyl chloride(PVC) and silicone sheets infused with or without known irritants resulting in the correct identification of the irritation potential of the materials. Around-robin study challenged the RhE models with compounds of known irritation potential embedded in common medical device polymers to further validate the in vitro method (De Jong et al. 2018). Like the Pellevosin et al.(2018) study, the round-robin also found that the RhE model could correctly classify the irritation potential of materials embedded with known irritants. De Jong et al.(2020) evaluated if the compounded-embedded polymers would have the same outcomes in the rabbit in vivo model and found a good correlation between the models. Additionally, the study also evaluated several medical device components and commonly used medical device materials in both assays demonstrating consistent results between them as well.
As final, finished medical devices are of ten comprised of various materials and use a wide range of manufacturing processes that could leave potentially irritating residues, the resulting extracts evaluated in irritation assays can be highly complex chemical mixtures and, in turn, may generate different results in in vitro than in vivo assays. With the release of ISO 10993-23:2021 and its inconsistent regulatory acceptance across geographical regions, a case study was conducted to understand how well the two assay types agreed. In this case study, final, finished medical devices were subjected to both in vitro and in vivo irritation assays to determine if the results correlated with each other. Additionally, as the in vitro irritation assay is an MTT based measurement, L929 cytotoxicity data were also evaluated to understand if in vitro cytotoxicity is predictive of in vitro irritation.