Join Mattek at SOT 2025


Mattek scientists will be attending and presenting posters at the Society of Toxicology Annual Meeting in Orlando, Florida. Our scientists are presenting 6 NEW POSTERS with new research, applications, and tissue models. Read more to see what we’ve been working on and request copies of our posters. We can’t wait to see you at SOT 2025!
Meet our team at Booth #1104
We’d love to chat: Schedule a Meeting
Poster Presentations:
NAM Based Prediction of Respiratory Toxicity using Human and Rat Airway Models (3228/G353)
Jo Wallace (1), Mary McElroy (1), Kalyani Guntur (2), Mitch Klausner (2), Seyoum Ayehunie (2)
1Charles River Laboratories, Edinburgh, UK, and 2Mattek Life Sciences, Ashland, MA
Session: New Approach Methods: In Vitro I | March 17, 2025 | 1:45 – 4:15pm
Abstract
Background: Human lung organotypic cultures are currently being used to assess direct toxicity of inhaled chemicals (OECD, 2022 and US EPA, 2023), however exact protocols are yet to be described in an OECD guideline. To achieve this aim and work within a tiered risk assessment (Andersen et al. 2019), we evaluated the acute toxicity and point of departure of a panel of chemicals with known inhalation risk assessment categories and specified point-of-contact toxicity in the lung. We determined the EC25 values in 2D and 3D human airway models (donor and passage matched epithelial cells) and a 3D rat airway epithelial model, across two laboratories (Charles River, UK and Mattek, USA) using harmonized protocols and SOPs. Methods: 10 chemicals were assessed in 2D monolayers of human airway epithelial cells and differentiated human EpiAirway (AIR-100-Day20) and rat EpiAirway (AIR-100-R) 3D tissue models. The assessed chemicals covered all human acute inhalation UN GHS hazard categories: Cat 1 (Isophorone diisocyanate), Cat 2 (potassium dichromate, methylisothiazolinone, benzalkonium chloride), Cat 3 (2-butyne-1,4-diol), Cat 4 (1,3-bis(aminomethyl) benzene) and Cat 5 (silica, lactose and propylene glycol). Chemical exposure was performed in two labs: Charles River (CRL) and Mattek (MTK) using a harmonized protocol. Each chemical was tested in each model at 6 concentrations (n=4 tissues/concentration) by direct (liquid) application to the apical surface of the tissue for 4 h, followed by 20 h recovery. Cell viability was assessed using transepithelial electrical resistance (TEER: 3D only) and alamarBlue (all) and the EC25 of each chemical was calculated by interpolation using the 2 concentrations which straddled 75% viability (EC25 = concentration which reduced the viability by 25% compared to the vehicle control). Results: 2D-human alamarBlue EC25s were highly reproducible between labs (within 2-fold) for 9/10 chemicals. The exception was isophorone diisocyanate, for which the difference was 5-fold. As expected, 2D-human monolayer cultures were more sensitive than 3D-human tissues for 9/10 chemicals (5 to 300-fold). 2-Butyne-1,4-diol was the only chemical which showed greater sensitivity in 3D tissues than the 2D monolayers (9-fold and 22-fold, respectively at CRL and MTK). For the 3D-human tissue model, the EC25s for 8/10 chemicals for alamarBlue and TEER were within 2.5-fold of each other when comparing CRL and MTK, indicating reproducibility between labs. 3D-human EC25’s generally ranked chemicals in the order associated with UN GHS acute respiratory hazard (scale of 1 to 5 with 1 being life threatening and 5 being non-toxic). Broadly, TEER EC25 ≤ 3 mg/mL predicted toxic materials (Cat 1-3), EC25 >3 mg/mL predicted Cat 4, and EC25’s > the highest tested concentration predicted Cat 5 materials (i.e. barrier function did not drop below 75% of the vehicle control exposed tissues). The results of alamarBlue were similar but less sensitive. Data from the 3D-rat model was similarly reproducible between labs, with 7 (alamarBlue) and 8 (TEER) EC25s being within 2.5-fold of each other when comparing CRL and MTK. EC25s for the rat model were slightly higher than EC25s from the human tissue. For the rat model, TEER EC25s ≤5 mg/mL indicated hazardous (Cat 1-3) and EC25s >5 mg/mL identified non-hazardous materials (Cat 4-5). Conclusion: The results confirm the general usefulness of the 2D model for setting the dose levels for further testing using 3D models. These initial results demonstrate that reproducibility between labs can be obtained with harmonized protocols and SOPs. The rat model is a useful tool to aid translation between in vivo rodent and in vitro human outcomes, and rat model data will be used in mathematical modelling to predict in vivo outcomes. Finally, the data show that this human EpiAirway protocol has the potential to allow prediction of human hazard classifications for acute inhalation risk. This work is part of a larger program which also includes repeat dose responses, aerosol vs liquid applications, and donor differences, with the eventual goal of generating a prediction model for inhalation risk of aerosol chemicals.
Worldwide Reproducibility of a Highly Differentiated 3-Dimensional Vaginal Tissue Model for Testing of Feminine Hygiene Products (3239/G364)
Mitch Klausner (1), Tim Landry (1), Kaitlyn Coen (1), Jan Markus (2), Silvia Letasiova (2), Kristina Kejlova (3), Marketa Dvorakova (3), Eliska Pacalova (3), Seyoum Ayehunie (1)
1Mattek Europe, Bratislava, Slovakia, 2Mattek Life Sciences, Ashland, MA, USA, 3Centre of Toxicology and Health Safety, National Institute of Public Health, Prague, Czech Republic
Session: New Approach Methods: In Vitro I | March 17, 2025 | 1:45 – 4:15pm
Abstract
Background: the toxicology test system is of extreme importance to regulators, in-house toxicologists, and formulation scientists. One of the advantages of in vitro test systems vis-à-vis animal-based systems is that the in vitro systems can be highly reproducible while in vivo models typically exhibit high variability. The commercially available, in vitro vaginal tissue model, EpiVaginal (Mattek Corporation) has been proposed as an in vitro replacement for the rabbit vaginal irritation test for assessing the safety of spermicides and other feminine care products (Costin et al., Toxicol In Vitro. 2020 Feb;62:104680. doi: 10.1016/j.tiv.2019.104680.). The EpiVaginal model is cultured using normal human vaginal epithelial cells, is highly differentiated, and develops a 3-dimensional structure that mirrors in vivo vaginal tissue. In the current study, reproducibility of the quality control data and testing results for feminine care products were each compared in 2 labs. Methods: For quality control purposes, bi-weekly batches of the vaginal model were assessed by exposing the tissue to the commonly used surfactant, Triton X-100 (1%), and the exposure time which reduced tissue viability to 50% (ET-50) was determined for each batch. The ET-50 batch release criterion was established in 2008, based on ET-50s for tissue lots produced in 2006-2007. In the current study, we investigated the reproducibility of tissue batches produced during 2024 in the US (n=20) and in Slovakia (n=8). To meet the lot acceptance criterion, the ET-50 for each lot must be in the range of 0.70 – 1.70 hrs. For testing of end-use products (test articles or TAs), tissues were produced by Mattek Europe (Bratislava) and testing was performed at Mattek Europe and at the Centre of Toxicology and Health Safety (Prague). Two concentrations of 5 feminine care products or ingredients were applied to the apical tissue surface for an exposure time of 24 hrs. After the 24 hr exposure period, tissue viability for the TAs was assessed using the MTT assay and transepithelial electrical resistance (TEER) measurements. Compared to the negative control tissues exposed to 100 µL of ultrapure water, values for %tissue viability (MTT) and %barrier integrity (TEER) were calculated. The results for the 2 labs were compared determining the difference in %tissue viability and %barrier integrity between the 2 labs. Results: For the 28 production lots analyzed in the US and Slovakia from January 1 to October 28, 2024, all ET-50s for 1% Triton X-100 were within the quality acceptance criterion, 0.70 < ET-50 < 1.70 hrs. In addition, the average coefficient of variation for the ET-50 dose response curves was 8.2%. The average difference for the %tissue viability for the 10 TAs was 10.1%; only 2 TAs had a difference >15%. The average difference for the %barrier integrity was 9.0%; only 2 TAs had a difference >15%. Conclusion: Long term stability of the EpiVaginal tissue was demonstrated by the ET-50 quality control results – all 28 lots of tissue met the lot acceptance criterion originally established in 2008. Excellent intralot tissue reproducibility was observed, based on the low average coefficient of variation for the ET-50 dose response curves (8.2%). Finally, a high level of interlab reproducibility was demonstrated in testing results for the tissue viability (MTT) and barrier integrity (TEER) assays which had average differences of 10.1% and 9.0%, respectively. The lot-to-lot and lab-to-lab reproducibility in two different geographical locations indicate that the vaginal model can serve as a valuable alternative method to screen feminine care products and reduce the use of animals.
Rapid Screening of the Gastrointestinal Toxicity Profile of Therapeutics Using an Automated Transepithelial Electrical Resistance (TEER) Measurement Device (3237/G362)
Kaitlyn Coen (1), Subhra Nag (2), Doug Bleau (2), Adrienne Watson (2), Mitch Klausner (1), Tim Landry (1)
1Mattek Life Sciences, Ashland, MA, USA, 2World Precision Instruments, LLC, Sarasota, Florida, USA
Session: New Approach Methods: In Vitro I | March 17, 2025 | 1:45 – 4:15pm
Abstract:
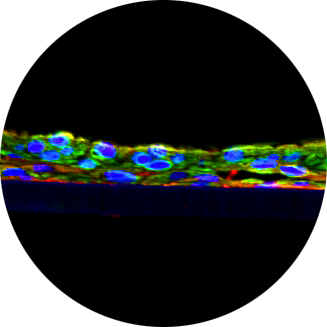
Background: Gastrointestinal toxicity (GIT) ranks among the most common clinical side effects for many orally administered pharmaceuticals, in particular for oncology drugs which are administered over an extended time period. Previously, we utilized an in vitro small intestine (SMI) microphysiological tissue model, EpiIntestinal™ (Mattek Corporation), which contains the epithelial cell types resident in the native human gastrointestinal tract, and transepithelial electrical resistance (TEER) measurements to evaluate the GIT profile of therapeutics and to predict oncology drug-induced diarrhea (Peters, et al., Toxicological Sciences, 2019 Mar 1;168(1):3-17). TEER is a non-invasive technique commonly used to monitor barrier integrity in 2D monolayers and 3D tissues. Daily TEER measurements were made over a six-week period, a typical therapeutic timeframe for oncology drugs, to monitor barrier integrity of 3D EpiIntestinal tissues grown on permeable membranes in 96-well insert plates. Manual TEER measurements were made on one tissue at a time, requiring 35-40 minutes to complete measurements for all 96 tissues. This manual method of measuring TEER limited the throughput of drug screening capabilities of the assay method, which is critical for the application of microphysiological systems in drug discovery and preclinical development. To overcome this challenge, we utilized the EVOMTM Auto instrument (World Precision Instruments), a high-throughput TEER measurement system, which can accurately and reproducibly measure the TEER of a 96-well plate in 4 minutes and 10 seconds. The EVOM Auto can be housed within a biological incubator or biological safety cabinet and run using a scheduled cycle mode, an additional feature that improves the ease of use. The EVOM Auto significantly increases the screening throughput, avoids technician fatigue, and increases the accuracy of TEER measurements by automating consistent measurement locations within the well. In this study, we investigated the ability of chemicals which cause short-term (ethylene glycol tetra-acetic acid, EGTA) and long-term (dextran sulfate sodium salt, DSS) reversible barrier disruption in the EpiIntestinal model as evaluated by automated TEER measurements and a Lucifer yellow permeability assay. Methods: Small intestine (SMI) epithelial cells were seeded onto PermaCell™ high pore density (0.4µm, 1.0×108 pores/cm2) PET membrane cell culture 96-well plates (Mattek), raised to the air liquid interface (ALI), and cultured for 2 weeks in specially formulated culture medium designed to induce differentiation. Barrier properties of the tissues were assessed using TEER. TEER was measured both manually with an EVOM Manual, and automatically using the EVOM Auto automated TEER measurement system. Automated readings were made with a read time of 2 seconds per well. Prior to TEER calculation, tissue sample resistance measurements were background subtracted using the resistance values of blank 100mM KCl buffer in the receiver plate of the 96-transwell assembly. Short-term (3 hour) exposure to EGTA was conducted using 1X Hank’s Buffered Salt Solution (HBSS) applied to the apical surface. Long term (10 day) exposure to DSS was conducted by adding DSS to the culture medium in both the apical and basolateral compartments. Reversible tissue damage assessed by TEER is expressed relative to the respective vehicle control tissues. Tissue samples were fixed for 3 hours in 10% formalin, permeabilized, and immunostained for Claudin 1 and DAPI. Images were acquired using an Olympus FV1000 confocal microscope. Permeability of the tissues was monitored using the Lucifer Yellow (LY) Permeability assay. 50µL of 100µM LY dye was applied to the apical surface and the basolateral receiver solution (RS) was replaced every 30 minutes for 2 hours. The LY concentration in the RS at each time point was determined using a fluorescence plate reader at an excitation bandwidth of 445-455nm, an emission bandwidth of 518-538 nm. Results: TEER measurements made using the EVOM Auto showed improved reproducibility and accuracy versus the manual readings. TEER for the 96 wells using the EVOM Auto averaged 162 ± 5.4 Ω*cm2 and TEER values remained steady over the 4 minutes and 10 seconds needed to measure all 96 wells. The manual readings averaged 155 ± 9.0 Ω*cm2 but values had a tendency to increase over the 24 minutes and 10 seconds needed to measure the 96 wells. Thus, the extended period outside the incubator for manual measurements causes changes in the TEER values while the EVOM Auto was more reproducible across the entire 96-well plate. Short-term (3hr) exposure to EGTA resulted in a dose-dependent response in TEER and LY leakage. TEER reduced significantly at 1, 3, 5, and 7 mM EGTA in HBSS and TEER values returned to baseline levels 48 hours after EGTA exposure was ended. Likewise, LY leakage increased significantly in the 5 mM and 7 mM EGTA treatment groups and returned to baseline following tissue recovery. Macroscopic (4x magnification) and microscopic (40x) immunostaining images showed tight junction protein Claudin-1 expression all culture conditions and treatment groups. Long-term exposure to DSS (1, 2.5, 5 and 10%) also resulted in a dose-dependent response in TEER and LY leakage. The highest dose (10%) showed significant tissue damage and decreased tight junction protein expression. Tissue damage at 1, 2.5, and 5% DSS was reversible following a 7-day recovery period and TEER returned to baselines levels post-recovery. The 10% DSS treatment group did not show TEER recovery but viable cells that remained following treatment showed monolayer reformation following the tissue recovery period. Conclusion: TEER measurements of the EpiIntestinal organotypic tissue model can be used to predict the GIT profile of therapeutics, and more specifically oncology drug-induced diarrhea, a common side effect of oncology drugs which can limit drug utilization. TEER is a non-destructive analytical technique which can be used to monitor changes to 2D and 3D tissues models and correlate in vitro and in vivo phenomena. The EVOM Auto, a new automated TEER measurement device, increases the screening throughput, avoids technician fatigue, and increases the reproducibility and accuracy of TEER measurements. The use of EGTA and DSS can be used to modulate the barrier function of the EpiIntestinal tissue model. Altered barrier function can be detected by TEER measurement and confirmed by LY permeability assay and immunostaining. The withdrawal of the EGTA and DSS allows the barrier to recover as verified by TEER measurement and LY permeability assay. We anticipate that the EpiIntestinal model together with the automated TEER measurement capabilities of the EVOM Auto will be very useful to screen the potential toxic effects of drug candidates in pharmaceutical development programs.
In vitro Assessment of Artificial Saliva and Complete Artificial Saliva in Oral in vitro Models (3236/G361)
Cao, X.(1), Farcas, M.T.(1), Prepelitskaya, Y.V.(1), Molignano, J.(2), Oldach, J.(2), Gutierrez, M.M.(1)
1Mattek Life Sciences, Ashland, MA, USA, 2Mattek Europe, Bratislava, Slovakia
Session: Late Breaking | March 20, 2025 | 9:15 – 11:45 AM
Abstract
Background and Purpose: Oral nicotine pouches (NPs) are tobacco-leaf-free oral nicotine products that are considered to be potential reduced-risk alternatives to tobacco-based products as part of a tobacco harm reduction paradigm. However, the toxicity profiles of these relatively new NPs, especially its local (oral) toxicity, are not well understood. Non-clinical in vitro studies have been conducted, including standardized Organization for Economic Co-operation and Development (OECD) genotoxicity tests and non-standardized mechanistic studies, to evaluate the toxicological characteristics of extracts from these products. Unlike combustible cigarettes, no standardized methods are available for extracting smokeless tobacco products for in vitro testing. For example, various solvents, such as phosphate-buffered saline (PBS), culture medium, enzyme-free artificial saliva (AS), and complete artificial saliva (CAS), have been used for extracting orally used products, including tobacco products. Among these solvents, CAS is a saliva substitute that closely resembles human saliva with most of its key components. Therefore, it is presumed to provide greater biological relevance compared to other solvents. To determine whether CAS is a more suitable alternative than AS for mechanistic testing, we conducted a vehicle control study to compare the extraction efficiency and a range of biological effects elicited by AS and CAS. Methods: The effects of extraction time and pouch cutting methods on extraction efficiency was first assessed to determine the optimal extraction parameters. Swedish style reference snus pouch CRP1.1 was used as a representative oral tobacco product. CRP1.1 was either cut in half or into fragments of approximately 4 mm in length and then extracted in AS for 2 h and 4 h at a concentration of 30% w/v. Extraction efficiency was measured based on nicotine and tobacco-specific nitrosamines (TSNAs) concentrations. To compare the extraction efficiency between AS and CAS, CRP1.1 was extracted in both AS and CAS (prepared as described by Chou and Que Hee1)at 10%, 20%, and 30% (w/v) and concentrations of nicotine and TSNAs (e.g., NAB, NAT, NNK, and NNN) quantified as measures for extraction efficiency. The biological effects of AS and CAS, including cytotoxicity, oxidative stress, and inflammation, were evaluated and compared at a range of concentrations in four in vitro oral models representing different levels of complexity, i.e., primary human gingival fibroblast (HGFs), human oral epithelial cells (HOEs), EpiOral model (ORL-200), and EpiOral-Full Thickness (ORL-300-FT) model. HGFs and HOEs were seeded on 96-well plates and exposed to four concentrations (5%, 10%, 15%, and 20% v/v) of AS and CAS diluted in respective media for 24 hours. ORL-200 and ORL-300-FT, which were cultured from the same donor as the HGFs and HOEs, were also exposed to four concentrations (20%, 50%, 80%, and 100% v/v) of AS and CAS diluted in TEER-buffer from the apical side for 24 hours. Cytotoxicity was assessed using the MTT assay. Response to oxidative stress was evaluated by 8-isoprostane ELISA. Pro-inflammatory response was measured using interleukin-8 (IL-8) and IL-6 ELISA. Results: Extraction efficiency as measured by nicotine and TSNA concentrations were comparable between AS and CAS extracts of CRP1.1 at the same w/v extract concentrations. Thus, neither the cutting size of the pouch nor the extraction duration (2 h vs. 4 h) had an effect on the extraction efficiency. However, extraction efficiency decreased with increasing w/v extract concentrations. Neither AS nor CAS induced significant responses in cytotoxicity and oxidative stress at any test concentration in the four in vitro oral models. However, both AS and CAS elicited significant concentration-dependent proinflammatory responses but exhibited different patterns. AS induced secretion of both IL-6 and IL-8 secretion in HOEs, but not in HGFs. CAS, on the other hand, increased IL-6 secretion in HGFs, but not in HOEs. It also caused the release of IL-8 in both HGFs and HOEs, with a higher level of induction in HOEs. Furthermore, AS and CAS did not induce significant proinflammatory responses in both ORL-200 and ORL-300-FT tissue models. Instead, AS, but not CAS, decreased the release of IL-6 in ORL-200 and ORL-300-FT and the release of IL-8 only in ORL-200. Conclusions: Conventionally, vehicle control effects are mainly assessed using assays that measure cytotoxicity. In this study, we demonstrated that AS and CAS caused significant release of IL-6 and IL-8 in HGFs and HOEs, despite the lack of measurable effects on cytotoxicity and oxidative stress. These findings highlight the importance of examining responses other than cytotoxicity when evaluating the baseline biological effects of vehicles for in vitro mechanistic testing. Based on our observations, CAS and ORL-300-FT were selected as the test system for future testing of oral tobacco products due to both the marginal vehicle control effect and their greater biological relevance.
Epi2SensA, a Gene Expression Assay with the EpiDerm Model to Predict Skin Sensitization in vitro (3236/G361)
C. Pellevoisin1,2, K. Guntur1, C. Romero1, T. Landry1, S. Letasiova3, and M. Klausner1
1Mattek Life Sciences, Ashland, MA, USA,2Urbilateria, Saint Cyrsur Loire, France, 3Mattek Europe, Bratislava, Slovakia
Session: New Approach Methods: Skin Sensitization | March 18, 2025 | 1:45 – 4:15pm
Abstract
Background and Purpose: In June 2024, the OECD updated Test Guideline 442D (OECD TG 442D) to include EpiSensA, a validated method using a reconstructed human epidermis (RhE) model for assessing skin sensitization. In parallel, the project for the me-too validation of the Epi2SensA method using the EpiDerm™ RhE model from Mattek was added to the OECD work plan. This poster presents the optimization and pre-validation of the Epi2SensA method with EpiDerm™ model conducted prior to the me-too validation started in 2024. Methods: Epi2SensA uses the reconstructed human epidermal model EpiDerm™ (EPI-200, produced by Mattek, Ashland, MA, USA, Mattek Europe, Bratislava, Slovakia, and Cellex Biotech, Shanghai, China). The principle of the test is to expose triplicate EpiDerm™ tissues topically to different concentrations of a test chemical. The gene expression of four markers associated with the keratinocyte response to the early phases of skin sensitization (induction of cytoprotective gene pathways and inflammatory responses) is evaluated by RT-qPCR. By comparing the fold induction of these genes with vehicle-treated tissues, it’s possible to classify the test articles as skin sensitizers or non-sensitizers. Potential cytotoxic effects of the test articles are evaluated by Lactate Dehydrogenase (LDH) quantification in the culture medium. For optimization of the protocol, this method was compared to cell viability measured by the MTT colorimetric assay. Results: The Epi2SensA protocol was adapted for the EpiDerm™ model from the validated reference method (VRM) with a limited set of chemicals. The method was optimized for the volume used for dosing, 10μL instead of 5μL, and the duration of exposure was reduced from 6 hours to 1h plus 5 hours of post-incubation. The concentration of Clotrimazol, one of the two positive controls, was modified from 0.78% to 1.56%. Optimization of the protocol led to a high reproducibility of the result for the controls tested over 10 independent runs. When evaluated against a set of chemicals including those from the VRM performance standards, Epi2Sensa was able to detect 6 of the 7 pre/pro haptens tested. It correctly classified 14/16 skin sensitizers, with 2 skin sensitizers classified false negative including Lauryl gallate, a pro-hapten also misclassified by the VRM. The method correctly classified 5 of the 6 non-sensitizers tested, including SDS, classified as false positive in the VRM. Conclusions: Adaptations of the protocol for Mattek’s EpiDerm model have optimized the method for reliable and reproducible results. Based on the set of chemicals tested, the accuracy of the method and its reproducibility with the EpiDerm RhE model met the requirements of the VRM performance standards. During the summer of 2024, the Epi2Sensa method was successfully transferred to 3 naive laboratories to perform the OECD “me-too” validation for inclusion in the OECD TG 442D.
A Novel Multi-Organ Tox Plate with Integrated Workflow for Drug-Induced Toxicity Studies
Joseph Finelli1, Martha Mayo2, Paul Keselman3, Kaitlyn Coen1, Alex Armento1, and Seyoum Ayehunie1,
1Mattek Corporation, 200 Homer Avenue, Ashland MA, 2Sartorius Corporate Research, Marlborough MA and 3Sartorius Corporate Research, Ann Arbor MI
Session: New Approach Methods: In Vitro II | March 19, 2025 | 9:45 – 11:45am
Abstract
Background: Advanced primary cell-based 3D human tissue models play a prominent role in chemical and drug toxicity screening and serve as an alternative to animal testing. 3D tissue culture systems are well-polarized and recapitulate the microenvironment of the in vivo counterpart. Currently, in vitro toxicological studies and dose-range finding experiments are performed using a single in vitro tissue or organ model system. In this study, we developed a multi-organ tox plate (MOTP) containing trio organs of intestine, liver, and kidney tissue models in a 96-well plate format. The MOTP was then integrated with high-throughput imaging and automated live-cell analysis. This allows dose-range finding experiments of a single or multiple drugs to be performed in parallel on three organ systems: 3D organotypic human intestine, kidney, and liver tissue models. Additionally, integrating the multi-tox plate with high-throughput accelerates data collection by enabling real-time measurement and automated EC50 calculations for test drugs. Methods: Cells representing three organ systems of intestine, liver, and kidney were seeded on a 96-well tox plate (32 wells per tissue type). Cells were cultured under submerged conditions (1-3 days) and air-lifted for 12 days to make them differentiate and stratify. To test the integrated workflow, we first reconstructed a single organ plate of the 3D human kidney model and dosed it with Cisplatin (kidney toxicant) and Oxaliplatin (non-toxicant) at different concentrations of each drug in the presence of the Incucyte® Cytotox green dye (Sartorius, Ann Arbor, MI) to monitor cell death. Following dosing, quantitative live-cell assays were performed by taking images every 4 hours for a total of 48 hours. The 50% drug-induced cell death (ET50) concentration was then calculated using the Incucyte® S3 live-cell analysis system (Sartorius) to capture cellular changes. Next, we expanded the study and developed a 96-well MOTP by reconstructing 3D tissue models of intestine, liver, and kidney on the same tox plate. To qualify tissues for drug testing, a pre-dose transepithelial electrical resistance (TEER) measurement was performed on all tissues on the tox plate, and tissues with TEER values of >90 ohms*cm² (intestinal), >100 ohms*cm² (kidney), and >80 ohms*cm² (liver) were used in the study. The tissues were then dosed with three model drugs: Fialuridine (liver toxicant), Cisplatin (kidney toxicant), and Troglitazone (liver toxicant) at 5 concentrations/drug using N=4 tissues/concentration/drug in the presence of a cell death marker, Cytotox Green. Dosed tissues were then incubated at 37°C and imaged in an Incucyte® Live-Cell Analysis System (Sartorius, Ann Arbor, MI) housed within the incubator. Green fluorescence images were acquired at 10X in real-time every 4 hours for a total of 48 hours. For each image, global mean fluorescence values were calculated using the Basic Analyzer module available with the Incucyte® instrument. At the end of 48 hours, TEER measurements were performed to monitor drug-induced acute organ toxicity. Results: Results of the pilot study showed a dose-dependent decrease in TEER following Cisplatin treatment of the 3D kidney tissue model. However, tissue barrier integrity was not affected when treated with Oxaliplatin. Data from the Incucyte® live-cell analysis showed the average ET50 values for Cisplatin was 17.25 µM, which is comparable with that obtained manually in previous studies. However, no drug-induced acute kidney injury was observed for Oxaliplatin-treated tissues at the concentrations tested. We then expanded the study to evaluate the toxicity potential of 3 test drugs, Cisplatin, Fialuridine, and Troglitazone on tissues growing on MOTP. The post-treatment TEER results showed that Cisplatin was toxic to all three tissue models, while the known human liver toxicant, Fialuridine, was specifically toxic to the liver but not to the small intestine or the kidney. Troglitazone was toxic to liver and kidney but not toxic to intestinal tissue. Analysis of the images taken at 4-hour intervals following exposure to Cisplatin showed a dose- and time-dependent decrease in TEER for all tissue types. However, tissues exposed to Fialuridine showed toxicity only on liver tissues but not on either the intestinal or kidney tissues. Conclusion: The integrated workflow can serve as a valuable tool for drug toxicity testing. The integrated trio-tox assay system is economical, accelerates in vitro drug toxicity assays, and ultimately reduces the use of animals in experimentation.
An in vitro Method for Assessment of Gastrointestinal Toxicity of Food Additive and Food Contaminant Nanoparticles
S. Ayehuni1, C. Pellevoisin1, J. Markus2, M. Klausner1, A. Helfrick1, A. Amento1
1 Mattek Europe, Bratislava, Slovakia, 2Mattek Life Sciences Ashland, MA, USA, 3Adriaens Consulting BVBA, Aalter, Belgium
Session: Late Breaking | March 20, 2024 | 9:45-11:45am
Abstract
Background and Purpose: The expanding use of nanoparticles (NPs) in various applications has raised concerns about their potential health effects, particularly when ingested via food, water, drugs, or cosmetics. In the food industry, there is increasing use of NPs in the food processing, packaging and directly in food products for their antimicrobial, nutrient, coloring and texture-enhancing properties. However, the toxicological impacts of NPs on the human gastrointestinal tract remain incompletely understood. We have developed an in vitro method using the reconstructed human model of the small intestine, EpiIntestinal, to evaluate acute and chronic effects of various NPs, including some food additives such as titanium dioxide (E171), iron oxide (E172),silver (E174), and gold (E175). The evaluation was done through multiple endpoints: barrier integrity, tissue viability, oxidative stress and inflammatory response. In addition, a permeation study was conducted to assess applicability of the EpiIntestinal to study systemic exposure to NPs from food industry. Methods: EpiIntestinal tissues were exposed to NPs (CuO, ZnO, SiO2, TiO2, Ag, Al, FeO, Au) at concentrations ranging from 5-900 μg/mL for 24 hours. Toxicity was assessed by measuring changes to barrier (TEER), tissue viability (MTT assay), histological analysis, cytokine release, oxidative stress (8-isoprostane release), and DNA damage (comet assay) The maximum tolerated dose (MTD), corresponding to concentrations with no acute toxicity(concentrations with less than 20% reduction in either TEER or MTT values), was estimated. In the second step, the EpiIntestinal model was exposed chronically to the MTD by repeated application every 48 hours for up to 18 days with TEER and MTT performed periodically. For the permeation study, 50 μLof polystyrene latex nanoparticles with red fluorophore were applied to the apical surface of the EpiIntestinal model and supernatants were collected from the basolateral compartment after 2hr, 4hr, 6hr, and 24hr. Permeated particles were quantified using a fluorescence spectrometer. Results: Following acute exposure, CuO, and ZnO, showed significant dose-dependent reductions in barrier integrity (TEER) and tissue viability (MTT). TheseNPs also induced histological damage and increased release of the pro-inflammatory cytokine IL-8. Analysis of culture supernatants showed a dose-dependent increase of 8-isoprostane release following exposure to CuO and a slight increase by ZnO, and FeO but not to Ag nanoparticles. Taking these results together, TiO2, Ag, Al, and FeO showed minimal acute toxicity at the tested concentrations. After repeated application at the MTD dose which induced no acute toxicity, a progressive reduction of cell viability is observed with CuO and to a lesser extent for TiO2, Au, FeO and, only at longer exposure time, with Al. No significant changes were observed with ZnO, Ag and Si. The flux of polystyrene latex nanoparticles through EpiIntestinal was calculated from permeation study: 1.03 ug/cm2/hr. Conclusions: Our results demonstrate that the EpiIntestinal model provides a physiologically relevant platform for assessing the potential toxicity effects of NPs present in the food. The exposure conditions, acute and chronic, and the different endpoints evaluated showed specific activity profiles depending on the NPs considered. Beyond local effects, the permeation study also suggests utilization of the EpiIntestinal model to assess the risk of deposition of nanoparticles at distant organs and systemic exposure to nanoparticles in the food industry.