Visit Mattek at the Society of Toxicology’s 58th Annual Meeting
Mattek will once again attend the Society of Toxicology annual meeting in Baltimore, MD, beginning March 10 and lasting through March 14, 2019. This year’s meeting will take place at the Baltimore Convention Center. The Society of Toxicology (SOT) has held its annual meeting in Baltimore before, most recently for its 56th annual meeting in 2017. Mattek will be presenting posters and exhibiting at booth #3420. If you’re attending too, be sure to stop by and say hello! Below is a list of all the posters we will be presenting at this year’s meeting, including when and where during the conference. Click the buttons to request a copy.
Visit Us at Booth #3420
View our posters:
Effects of Ammonia Vapor Exposure on Viability in a Full-Thickness Human Skin Tissue Model Abstract 2432 Poster No. P847
Tuesday Morning, March 12 Author Attended 10:45 am to 12:15 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models I 9:15 am to 4:30 pm
J. Molignano1, M. Bachelor1, P. J. Hayden1, H. D. Garcia2, K. Toon3, and V. E. Ryder3. 1Mattek Corporation, Ashland, MA; 2KBRWyle, Houston, TX; and 3NASA Johnson Space Center, Houston, TX.
In this study, EpiDermFT, an in vitro 3D model of human skin, was used to evaluate the effects of ammonia vapor on skin to simulate in vivo exposure. The US Segment of the International Space Station (ISS) utilizes ammonia in the external loops of the active thermal control system. There is a low likelihood failure scenario that would allow ammonia to enter the habitable volume of the ISS via the interface heat exchangers. Protective masks have been developed to protect the eyes and respiratory tracts of crew in the event of a breach, but the dose/response for the effects of elevated ammonia vapor concentrations on intact human skin is largely unknown. Since EpiDermFT is cultured at the air-liquid interface and is amenable to topical exposures of test material, this 3D tissue model was an appropriate test system to simulate in vivo exposure to ammonia vapor. A custom exposure device was developed by Vitrocell and engineered to expose the apical surface of EpiDermFT tissues to either clean air (as a control) or ammonia gas at concentrations of 10, 100, 1000, 10,000, 30,000 or 50,000 ppm for 1, 5 or 20 minutes. Tissues were assessed immediately following exposure or 24 hours post-exposure for cell viability using the MTT assay and for morphological changes indicative of toxicity. Data indicate that concentrations between 10-1000 ppm ammonia for up to 20 min did not have an immediate or delayed (24 hr) effect on dermal tissue viability. Signs of toxicity, especially 24 hr post-exposure were noted at 10,000 ppm ammonia and increased in severity with both increasing exposure time and concentration. To our knowledge, this report represents the first evaluation of ammonia vapor on skin. Altogether, we demonstrate the utility of the EpiDermFT model as a relevant substitute of human skin for evaluation of cytotoxicity in response to environmental insults.
Request Poster
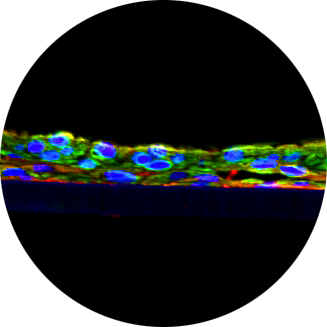
Molecular Footprints of Oxidative Stress in Corneal Injuries of Different Origin: Utilization of Human Organotypic 3D Corneal Tissue Model Abstract 2450 Poster No. P865
Tuesday Morning, March 12 Author Attended 10:45 am to 12:15 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models I 9:15 am to 4:30 pm
Y. Kaluzhny, M. Kinuthia, T. Truong, A. Lapointe, M. Klausner, and P. Hayden. Mattek Corporation, Ashland, MA.
Oxidative stress (OS) plays an important role in many corneal injuries (CI), including chemical burns, UVB irradiation, and exposure to vesicating agents. Current methods used to investigate mechanisms of CI utilize monolayer cell cultures or animals that result in poor data extrapolation and standardization, low throughput and high cost. Physiologically relevant, human-based in vitro models for ocular research are needed. This study evaluated the utility of an in vitro reconstructed 3D tissue model (EpiCorneal) to study molecular mechanisms of OS corneal damage. The constructs are comprised of normal human corneal epithelial cells that are cultured at the air-liquid interface, develop a tight barrier (TEER 1000±250 Ω*cm2), express tight junctions, mucins, and key corneal detoxification enzymes similar to in vivo human cornea. OS was generated by exposure to 60/120 mJ of UVB, topical application of 20/50 mM of hydrogen peroxide (HP) for 2h or 1.5 mg/ml of nitrogen mustard (NM, warfare agent) for 10/30 min. Barrier function, tissue viability, reactive oxygen species (ROS), lipid oxidation, cytokine release, histology, and gene expression were evaluated after 2/24h post-exposure. HP reduced tissue barrier to 50% and viability (MTT assay) to 70% after 2h incubation compared to negative control (NC). NM reduced tissue barrier to 72%, however tissue viability was not affected after 2h. 20 mM HP- and 10 min NM-treated tissues recovered after 24h, while 50 mM HP- and 30 min NM-treated tissues degenerated as confirmed by TEER, MTT assay, LDH release, and histological analysis. UVB irradiation didn’t have an effect on tissue barrier, viability, and LDH release, but intracellular ROS increased by 17X when compared to the NC. The highest lipid oxidation (20.1X increase) and IL-8 release (18.6X increase) relative to NC were observed for 10min/NM-treated tissues at 24h post-treatment. Utilizing a PCR gene array we compared effects of different CI corneal injuries on the expression of 84 OS responsive genes, and found a specific molecular footprint for each mechanism of corneal injury. In summary, the in vitro reconstructed human corneal tissue model structurally and functionally reproduced key features of in vivo corneal tissue. Unique toxicity and molecular responses were revealed for various types of ocular damage. This model is anticipated to be a useful tool to study molecular mechanisms of corneal damage and to evaluate new corneal drug formulations.
Request Poster
Validation of an In Vitro Alternative Method for Acute Respiratory Toxicity Testing Abstract 2461 Poster No. P876
Tuesday Afternoon, March 12 Author Attended 1:30 pm to 3:00 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models II 9:15 am to 4:30 pm
M. Debatis, G. R. Jackson, A. Maione, M. Klausner, and P. J. Hayden. Mattek Corporation, Ashland, MA.
Determination of acute respiratory toxicity potential is important for establishing safe use of chemicals and consumer products. Inhalation toxicity testing and classification procedures currently accepted by worldwide government regulatory agencies require the use of tests based on lethal effects in animals. The current work provides an update on the development and validation of an alternative non-animal method for determining acute respiratory toxicity using the EpiAirway™ in vitro human airway model. The in vitro test method exposed EpiAirway tissues to four concentrations of test chemicals for three hours via apical application using either aqueous or corn oil vehicles. After the initial three hour exposure, the test chemicals were rinsed off and the tissues were incubated for an additional 21 hours. A variety of endpoints were evaluated including tissue viability (MTT assay), barrier function (transepithelial electrical resistance: TEER), glutathione content and cytokine secretion (IL-8, IL-6, IP-10, GM-CSF, RANTES, MIP-1β, Il-1α, TNF-α). Seventy-five chemicals with known in vivo inhalation toxicity effects, and covering a broad range of toxicity classes, chemical structures and physical properties, were evaluated. The in vitro toxicity data were utilized to establish a prediction model to classify the chemicals into categories including: highly toxic/corrosive, moderately toxic and mild/non-toxic. The data demonstrate that the EpiAirway acute respiratory toxicity test using the MTT viability assay endpoint is highly sensitive for identifying respiratory toxins/corrosives. TEER, glutathione content and cytokine secretion endpoints were less informative. Corrosivity and electrophilic and oxidative reactivity appear to be the predominant mechanisms of toxicity for the most highly toxic chemicals identified in the EpiAirway test. These results indicate that the EpiAirway test using the MTT viability endpoint is a promising alternative to animal tests for the assessment of acute respiratory toxicity.
Request Poster
Development of a Chronic Respiratory Toxicity Assay Using an In Vitro Human Airway Model Abstract 2762 Poster No. 877
Tuesday Afternoon, March 12 Author Attended 1:30 pm to 3:00 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models II 9:15 am to 4:30 pm
G. R. Jackson, M. Debatis, A. G. Maione, M. Klausner, J. Oldach, and P. J. Hayden. Mattek Corporation, Ashland, MA.
Knowledge of chronic respiratory toxicity potential is important for establishing safe use of chemicals and consumer products. The current work describes efforts to develop an alternative, non-animal method for determining chronic respiratory toxicity using the EpiAirway™ in vitro human airway model. Initial acute toxicity experiments were conducted by exposing EpiAirway tissues to four concentrations of test chemicals via apical application using either aqueous or corn oil vehicles for three hours. After exposure, the test chemicals were rinsed off and the tissues were incubated for an additional 21 hours. An IC75 concentration (concentration required to reduce the endpoint value to 75% of vehicle exposed controls) was determined from the dose-response data using barrier function (determined by measuring transepithelial electrical resistance (TEER)) and tissue viability (MTT assay) as endpoints. Based on the determined IC75 value, EpiAirway tissues were exposed to six serial dilutions of the test chemicals, using the IC75 as the highest dose. Tissues were apically exposed for three hours, followed by rinsing, every Monday, Wednesday and Friday, with TEER measured prior to each dose application. Experiments were continued for at least 30 days to determine no-observed-adverse-effect level (NOAEL) doses. Experiments conducted with formaldehyde, ethanol and dimethylacetamide found NOAEL values of 0.0001, 0.5 and >0.5 mg/ml, respectively. Expansion of the data set to include chemicals of different classes, chemical structures and physical properties is ongoing. These results indicate that in vitro airway tissue models using TEER as a convenient non-destructive endpoint are a promising alternative to animal tests for assessment of chronic respiratory toxicity.
Request Poster
Development and Characterization of an In Vitro Human iPSC-Derived Neurospheroid Model Abstract 2474 Poster No. 889
Tuesday Afternoon, March 12 Author Attended 1:30 pm to 3:00 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models II 9:15 am to 4:30 pm
J. L. Mohn, M. Klausner, and P. J. Hayden. Mattek Corporation, Ashland, MA.
Multiple approaches have recently been described to generate in vitro neural organoid models from human induced pluripotent stem cells (iPSC). While these models are effective at recapitulating many features of human fetal brain development, the processes used to generate them are not amenable to large-scale production and high-throughput applications. The goal of this exploratory research is to develop a scalable and reproducible in vitro, 3-dimensional neurospheroid model that may be used for high-throughput applications assessing neurodevelopmental toxicology (DNT) and drug development. Methods: Neurospheroids were generated by seeding iPSC-derived neural progenitor cells (NPCs) in ultra-low adhesion multi-well plates. Neuronal differentiation was induced with medium containing BNDF and GDNF. Neurospheroids were maintained in culture for up to 8 weeks. Immunofluorescent analysis of neurospheroids was performed on frozen sections and gene expression was assessed using real-time quantitative PCR (qPCR). This approach yielded neurospheroids of consistent size over time, both within and across batches. Immunofluorescent analysis of frozen neurospheroid sections revealed widespread expression of neuronal markers MAP2 and βIII-tubulin, as well as VGLUT1, indicating presence of presynaptic glutamatergic specializations. qPCR analyses showed increases in expression of neuronal genes including MAP2 and synaptophysin over time, while expression of progenitor markers (SOX2, nestin) decreased. Neurospheroids of consistent size containing mature neurons were successfully generated using this approach. The model is easily scalable and can be adapted to either 96- or 384-well plate formats, allowing use in high-throughput applications. Further efforts will use this platform to establish assays measuring cellular toxicity and processes modeling DNT. Neurospheroid complexity will also be improved by the incorporation of additional cell types such as astrocytes and microglia.
Request Poster
Evaluation of Drug Bioavailability and Biocompatibility Using an Organotypic Human Corneal Tissue Model Abstract 2481 Poster No. P896
Tuesday Afternoon, March 12 Author Attended 1:30 pm to 3:00 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models II 9:15 am to 4:30 pm
Y. Kaluzhny, M. Kinuthia, T. Truong, A. Lapointe, M. Klausner, and P. Hayden. Mattek Corporation, Ashland, MA
Assessment of corneal drug penetration is crucial for development of effective ophthalmic medicines. Current studies utilize excised animal corneas that are not suitable for rapid drug screening, have poor species extrapolation and standardization. Physiologically relevant, human-based in vitro models for development of new ophthalmics are needed. This study evaluated the utility of an in vitro reconstructed tissue model (EpiCorneal) to study ophthalmic drug delivery. The model contains normal human corneal epithelial cells that grow at the air-liquid interface and develop a tight barrier (TEER 1000 ±250 Ω*cm2) that is comparable to the in vivo human cornea, express tight junctions, mucins, and key corneal detoxification enzymes. The performance of the reconstructed corneal tissues was demonstrated using formulations of known antiglaucoma drugs. The effect on drug absorption, tissue viability (MTT assay) and integrity (TEER, LY leakage) was investigated after 0.5h and 2h treatments and compared to the tissues treated with the Krebs-Ringer buffer (KRB). Steady-state flux reached by latanoprost (LAT) in commercial formulation and LAT in KRB was 3.47 and 2.04 nmol/(cm2·h), and Papp was 2.50×10-5and 1.47×10-5 cm/sec, respectively. Flux for bimatoprost (BIM) in commercial formulation (Lumigan) and BIM in KRB was 18.33 and 3.43 nmol/(cm2·h), and Papp was 5.58×10-5 and 1.04×10-5 cm/sec, respectively. Flux reached after application of free acid metabolites of LAT/BIM in KRB was 0.18/0.53 nmol/(cm2·h), and Papp was 1.22×10-6/1.85×10-6 cm/sec, respectively. Incubation with commercial LAT/Lumigan for 0.5h resulted in a 1.8/3.2-fold increase in tissue leakage and a decline in TEER to 42.2/ 44.1%; additionally, tissue viability declined to 71.0/74.2% after 2h. All other eye drop formulations did not have an effect after 0.5h; however, 2h exposure reduced TEER to 65.7%/77.8% for LAT/BIM. Both commercial formulations contained 0.02% Benzalkonium Chloride (BAC) as a preservative. By itself BAC at concentrations 0.005% and 0.01% in KRB did not have an effect on 3D tissues; however, at 0.02% it reduced TEER to 51.6%; and 0.04% – reduced TEER to 18.3%, increased LY leakage (3.5%), and reduced viability to 43.8%. In summary, the EpiCorneal model demonstrated high predictive capabilities for drug bioavailability/biocompatibility of various known ophthalmic formulations/excipients. The tissue model may be useful for evaluation of corneal drug permeability and safety during the development of new ophthalmics.
Request Poster
Organotypic In Vitro Human Airway Models Can Recapitulate Aspects of Pulmonary Fibrosis Abstract 2482 Poster No. P897
Tuesday Afternoon, March 12 Author Attended 1:30 pm to 3:00 pm CC Exhibit Hall Poster Session: Alternatives to Mammalian Models II 9:15 am to 4:30 pm
A. G. Maione, G. R. Jackson, O. O’Connell, J. Foisy, M. Klausner, and P. J. Hayden. Mattek Corporation, Ashland, MA.
Pulmonary fibrosis (PF) is a debilitating, typically fatal condition that may be caused by a variety of factors, including occupational and environmental exposures, drugs such as amiodarone and bleomycin, radiation exposure, and genetic predisposition. However, in 20-30% of cases the cause is unknown (i.e. idiopathic pulmonary fibrosis, IPF). Currently approved IPF drugs (pirfenidone, nintedanib) have only limited efficacy, and lung transplantation remains the best treatment option for IPF patients. Despite intense research, many of the molecular mechanisms involved in the initiation and progression of IPF remain unknown. Current IPF research relies on animal models and ex vivolung tissues, which are expensive and are not always predictive of clinical trial results. Currently available in vitro models produced from immortalized cells also do not adequately replicate IPF. The goal of the current work is to develop in vitro organotypic, 3D airway models from primary human cells which can be used to study IPF. In vitro models composed of differentiated primary human bronchial or alveolar epithelial cells and pulmonary fibroblasts were cultured at the air-liquid interface to replicate the in vivo microenvironment. The tissue models were treated with 10 ng/mL transforming growth factor beta (TGF-β) for at least six days to induce a fibrotic phenotype. Tissues were assessed for changes in morphology, expression of pro-fibrotic markers, extracellular matrix (ECM) production and barrier function. Treatment with TGF-β induced changes characteristic of PF, including increased expression of alpha-smooth muscle actin, Type III collagen and vimentin protein in the stromal compartment. In addition, qRT-PCR revealed increased mRNA expression of other fibrotic markers; matrix metalloproteinase 2, fibronectin and Type III collagen. By recapitulating aspects of PF, these co-culture tissue models provide an experimental system to study the cross-talk between the epithelium and fibroblasts, which is believed to be a key factor in PF development. Furthermore, these models can be utilized to investigate the molecular events contributing to pulmonary fibrosis and to evaluate new therapeutic agents.
Request Poster
Reconstruction of a Novel Primary Human Cell-Based 3D Colon Tissue Model Abstract 3064 Poster No. P601
Wednesday Morning, March 13 Author Attended 9:15 am to 10:45 am CC Exhibit Hall Poster Session: Emerging Technologies 9:15 am to 4:30 pm
A. Armento1, S. Bogojevic1, T. Landry1, M. Klausner1, P. Hayden1, and S. Ayehunie1. 1Mattek Corporation, Ashland, MA.
The purpose of this study was to reconstruct a primary human 3D colon tissue model that can be used for 1) microbiome studies, 2) screening of colorectal care products for their irritation potential, 3) safety and efficacy studies of anti-microbial products and 4) inflammation studies in the colorectal microenvironment. In this study, we characterized the structural features of a novel in vitro tissue model reconstructed from normal human primary colon epithelial cells and fibroblasts. Primary cells were expanded in monolayer culture and seeded onto microporous membrane inserts to reconstruct 3D organotypic colon tissues. The tissues were characterized for polarity of epithelial cells (H&E staining), epithelial and fibroblast cell markers (fluorescence confocal microscopy), and barrier integrity (transepithelial electrical resistance, TEER) measurement. Analysis of the 3D colon tissue model revealed: 1) wall-to-wall tissue growth by day 4; 2) epithelial cell morphology similar to human colon; 3) a physiological TEER value of >300 Ω*cm2 mimicking the colon microenvironment; and 4) expression of CK19 (epithelial cell marker), vimentin (fibroblast cell marker), and Alician blue PAS staining (mucous producing goblet cell marker) on the villi-like structure. When mixed epithelial cells and fibroblasts are seeded on tissue culture inserts, there was a self-assembly pattern of differentiation in which the fibroblasts occupy the base layer and the epithelial cells differentiate and stratify on the apical layer. This new human cell-based colon tissue model will be a useful tool for pre-clinical assessment of microbiomes, mucosal inflammation, and screening of colorectal care products for their irritation potential. Such models will also reduce the use of animals for experimentation.
Request Poster
Modeling of Ligand-Induced Acute and Chronic Inflammation in the Gastrointestinal Tract Using In Vitro 3D-Human Small Intestinal Tissues Abstract 3046 Poster No. P513
Wednesday Morning, March 13 Author Attended 9:15 am to 10:45 am CC Exhibit Hall Poster Session: Inflammation 9:15 am to 4:30 pm
S. Ayehunie1, J. Markus2, T. Landry1, Z. Stevens1, A. Armento1, M. Klausner1, and P. Hayden1. 1Mattek Corporation, Ashland, MA; and 2Mattek IVLSL, Bratislava, Slovakia.
The intestinal epithelium is known to be involved in innate immune responses by recognizing potential pathogens through cellular pattern recognition receptors (PRRs). The purpose of this study was to investigate PRR responses following exposure of an in vitro 3D human small intestinal (SMI) microtissue to various Toll-like receptor (TLRs) and Nod-like receptor (NOD) ligands. The SMI microtissues were cultured using human intestinal fibroblasts and enterocytes and their 3-dimensional polarity and morphology mimics that of native in vivo tissues. Characterization of the microtissues included evaluation of structural features, barrier properties, and expression of drug transporters and drug metabolizing enzymes. Results showed that exposure of intestinal microtissues to live bacterial or ligands to TLR4 (lipopolysaccharide; LPS) and NOD2 (Muramyl dipeptide; MDP) were able to induce gene expression of proinflammatory cytokines such as IL-1β, IL-6, and RANTES. Prolonged exposure of intestinal microtissues to IL-1β resulted in reduced membrane integrity and induction of pro-inflammatory cytokines (IL-6 and CCL20) known to stimulate acquired immune cell responses by inducing cytokine release such as TNF-α and IFN-γ or by initiating the migration of inflammatory cells. These responses may be precursors for Inflammatory bowel-like disease (IBD). To simulate the effect of immune cell responses on the intestinal epithelium, we exposed the microtissues to IL-1β, TNF-α, and IFN-γ, which resulted in the reduction of membrane integrity and the release of proinflammatory cytokines. The effect of TNF-α and IFN-γ on the intestinal epithelium was further exacerbated if antigen-presenting cells such as dendritic cells were incorporated into the 3D intestinal microtissues. In summary, our results suggest that the EpiIntestinal tissue is capable of modeling innate immune responses and can be a useful in vitro tool to study the complex interactions of human intestinal epithelium with the microbiome in the induction of IBD-like disease.
Request Poster